Depressionsportalen
Depressionsportalen

Välkommen!

Utbildningar
Utöka dina kunskaper om depression med våra utbildningar

Föreläsningar
Här hittar du aktuella och tidigare föreläsningar inom depression.

Nytt om depression
Nya rön om svårbehandlad
depression och olika aspekter av behandling.

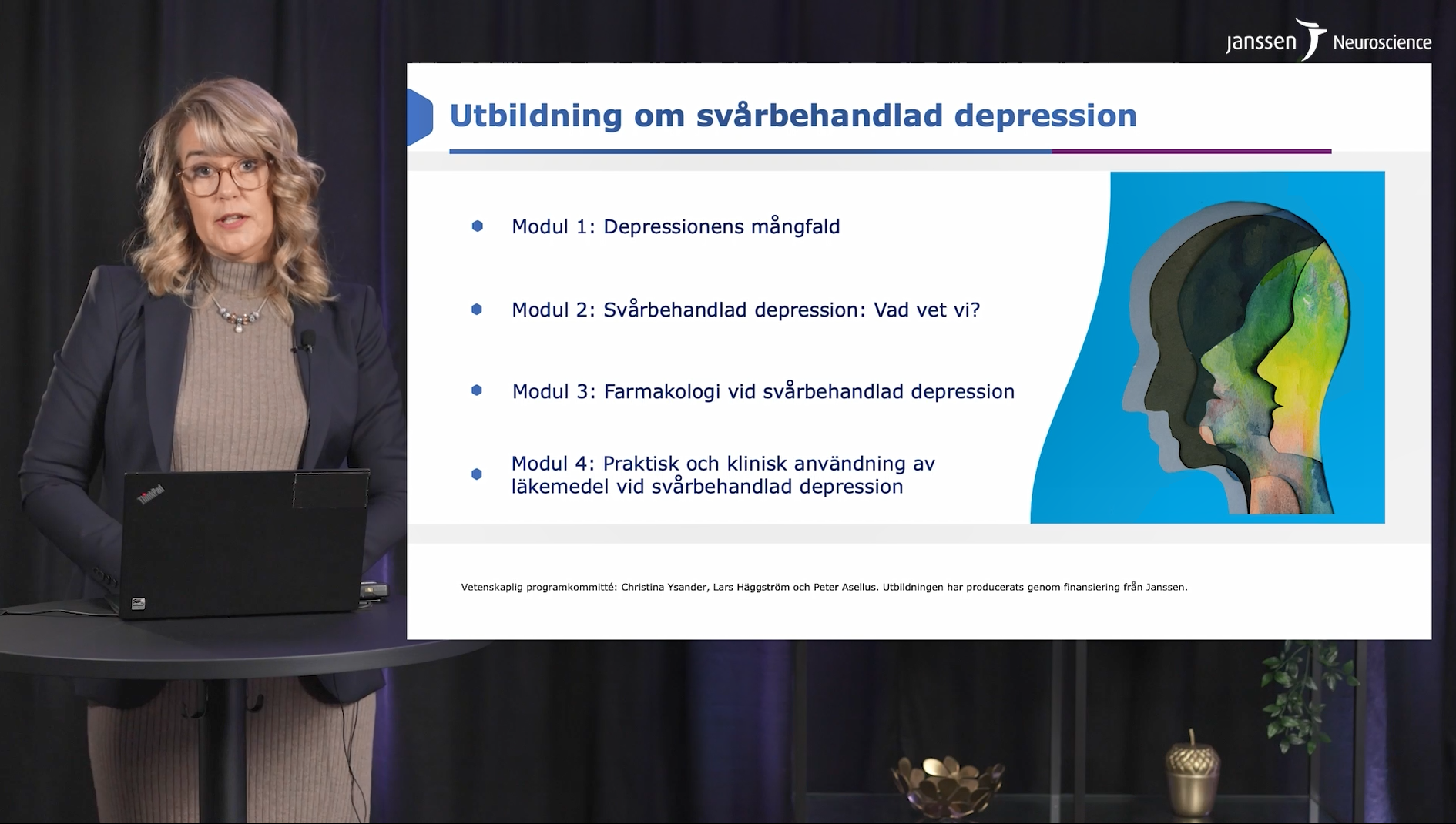
Svårbehandlad depression
Här hittar du utbildningar och videor om olika aspekter av svårbehandlad depression.
Nyhetsbrev
Nyhetsbrev
Prenumerera på de senaste nyheterna inom ditt specialistområde.


Studier
Här kan du läsa sammanfattningar av viktiga studier om svårbehandlad depression samt länkar till de fullständiga publikationerna.

Våra läkemedel
Läs mer om våra läkemedel inom depression.

Kontakt
Har du frågor och vill veta mer om svårbehandlad depression är du välkommen att kontakta oss i Janssen-teamet.
EM-92181 -